I Am in the midst of a real mental dilemma here.
For the last several years I have expressed to various parties and in multiple forums my interest in gastroenterology as a subspecialty in internal medicine. I find that dealing with the complications of liver failure, inflammatory bowel disease and similar digestive complaints to be among the medical cases I am most fascinated in. I love the procedural aspect of GI, endoscopies and colonoscopies feeling like some hi-tech medical video game. I love that GI is one of the nicer lifestyle specialties in internal medicine, and if I were to succeed in it, I would financially be pretty much set for life following the completion of my fellowship.
However, GI is among the most competitive subspecialties, right up there with cardiology, and critical care. Similar to my applications to medical school and then residency, there are always more people than positions available.
A Key component of Fellowship is academic medicine, i.e. research. The emphasis is on projects that explore new hypotheses although case reports and meta-analyses/reviews of existing studies is also encouraged and accepted.
And therein lies the rub.
I detest research. I have absolutely no interest in it whatsover whether it be benchwork, clinical studies, chart review, etc. The sum entirety of my interest in and love for medicine is all clinical. I like seeing patients, going to clinic, rounding in the hospital and basically making a 9-5 living (although realistically medicine is never a 9 to 5, I think you get the gist). Once I leave the hospital, I honestly stop thinking about everything that is going on in it. I have other interests. I enjoy cooking, performing stand up comedy, riding motorcycles, a whole slew of non medically related activites.
Yet in order to successfully secure a fellowship position, I must have something published by the time I apply, or at the very least be involved in several projects I can talk about during my interviews.
I have told myself in the past that my love for the field is strong enough to put up with just enough research to get me the fellowship position, that once I make it, I can just have a clinical practice and its worth the sacrifice. I got myself involved in several projects beginning my intern year doing things like chart review and data entry on cirrhosis patients, who academically I find fascinating.
But I am beginning to wonder if I cant keep lying to myself like this. I really dont like even the minimal amount of research work I have forced myself to get involved in. And if by some lucky stroke of fortune I manage to secure a fellowship position anywhere in the country, the emphasis is going to be, at the very least, another 3 years of constant research and publishing before I can find a job just doing clinical work and never have to worry about publishing anything ever again. And I am beginning to realize I have serious doubts about my ability to stay motivated through that path.
The alternative option would be for me to become a hospitalist, an internal medicine doctor who deals strictly with patients in the hospital managing a multitude of problems from every organ system. Sure I would take a paycut in the long run (avg income for hospitalist is 150-180 thousand versus 200-250 thousand for a gastroenterologist) but I would also be able to start working soon as I finish residency in another 2 years without an additional 5 years of training, without the need to ever do research and pretty much avoiding academic medicine entirely.
I have things I want to do with my life still-I want to open my own restaurant, I want to continue traveling the world, I want to not still be some form of student when I am approaching my 40's. I can accomplish these goals no matter what choice I make, only the timetable and perhaps a few lifestyle choices are affected.
Of course, the majority of my friends and colleagues have heard me talk about GI from day one. Now while there is no shame and only minimal loss of face in changing my mind at this point, I of course have to wonder, would I be changing my mind for the right reasons.
Everyone has aspects of their job they dont like-am I overdramatizing this one feature and cheating myself out of a career I could really love? Or am I saving myself from 4 years of jumping through hoops when I could be just as happy doing none of the circus tricks required to do the kind of medicine I want to do? And if I do decide not to apply, what then do I tell to the colleagus and coworkers I have just spent the last year convincing I want to be in the field?
Any other resident/fellow/subspecialists out there, I could really use your thoughts on this if you have been in a similar situation
And the remainder of my xanga readers, what is your input?
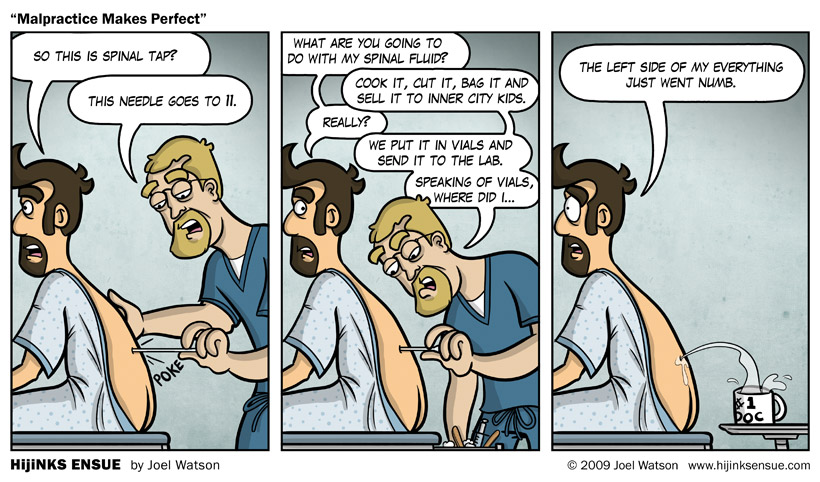
The whole thing has left me with mental knots in my stomach


Recent Comments